In the womb, a fetus's digestive system is squeaky clean. After birth, a baby is exposed to microbes which quickly colonize its gut. After only one year of age, a baby has already attained a complex community of intestinal flora comparable to that of a full-grown adult.
A long-standing relationship
Research in recent years has shown that humans actually have a mutualistic relationship with their gut microbes – that is, a partnership in which both sides benefit. Our microbes receive housing and nourishment in our bodies. In return, they help us digest food, they regulate our immune system, and they produce hormones and neurotransmitters.
These effects of the gut microbiome on the rest of the body are so important that it is often referred to as the “forgotten organ.†Indeed, the number of microbes in our GI tract is equal to the number of human cells in our entire body!
Gut microbes produce digestive enzymes absent in human cells and help us to break down certain polysaccharides (carbohydrates). In turn, our gut flora community is affected by our diet. People fueled by a diet high in fat and protein tend to have a microbiome dominated by Bacteroides species, which specialize in breaking down plant starches and fibers. People eating high levels of carbohydrates show a majority of Prevotella species, bacteria associated with consumption of simple sugars.
Humans have housed microbes in their gastrointestinal tract for a long, long time. Indeed, many of these microbes have actually co-evolved with us. To boot, non-human primates such as bonobo apes and chimpanzees house many of the same bacteria that we do. This close human-microbe relationship can prove useful to studies of early human movement. For example, the bacterium Helicobacter pylori has been used to track migration of early Homo sapiens leaving Africa.
Gut flora influence metabolism
Researchers have found that the species composition of the gut microbiota influences metabolism and can have implications for obesity, glucose intolerance, and diabetes. In a landmark experiment, mice were fed diets supplemented with microbes from the stomachs of thin versus overweight humans. Apart from the microbial supplements, the two diets were identical. The mice that ingested microbes from the guts of obese humans gained a significant amount of weight in the weeks following the treatment, while those receiving microbes from slim humans remained unchanged.
Likely inspired by this study, Dr. Elaine Yu of Massachussetts General Hospital recently began running a series of tests to examine whether overweight people will slim down when given pills containing freeze-dried poop of skinny folks. These unsavory capsules contain enough bacteria to recolonize the patients' stomachs, changing the microbial community to one that may promote weight loss.
Artificial sweeteners affect gut microbes
Have you ever heard the baffling statistic that people who consume diet drinks tend to weigh more than those who drink the regular stuff? Turns out the explanation for this may lie in the gut microbiome.
Israeli researchers found that mice fed artificial sweeteners develop high blood sugar levels over time, indicating that their cells have begun to develop glucose intolerance. In humans, glucose intolerance is a precursor to diabetes and often coincides with obesity. Control group mice fed natural sugars in place of artificial sweeteners maintain normal blood sugar levels.
The researchers found they could actually reverse the glucose-intolerant condition of the mice fed artificial sweeteners. They first gave the mice antibiotics to completely clear the bacteria in their guts, then started the mice back on a normal diet lacking any sweetener. The mice became healthy again; their blood sugar levels gradually dropped to normal.
The same research team found that human test subjects introduced to a diet containing artificial sweeteners also begin to show a decreased cellular response to glucose, alongside a sharp change in the makeup of their gut microbiome community.
It seems that artificial sweeteners induce a change in the microbiome makeup which promotes glucose intolerance, but which is reversible upon antibiotic treatment to kill the “bad†microbes responsible for the worrisome condition.

Gut flora behave like a second brain
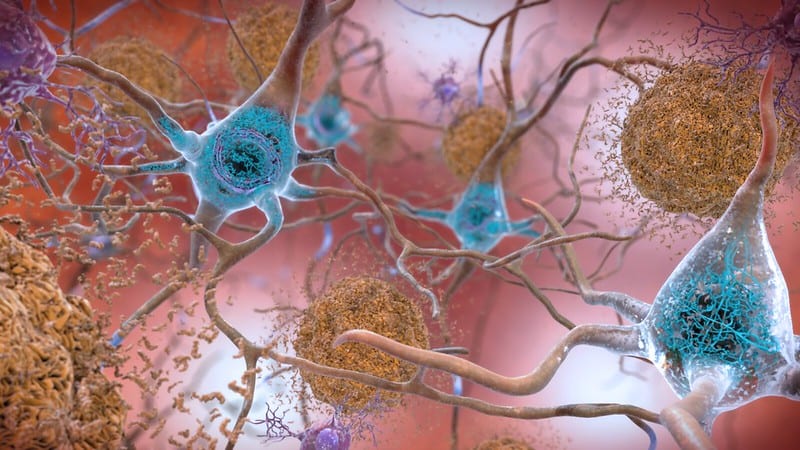
Not only does our “forgotten organ†have some control over our metabolism, it also may strongly affect our mood – thus its additional moniker as our “second brain.†The digestive system and the brain are linked in what is called the gut-brain axis.
The microbes in our gut synthesize a wide range of neurotransmitters, including serotonin, histamine, acetylcholine, and dopamine. Imbalances in these molecules can cause depression, memory loss, a weakened immune system, and insomnia.
The population of gut microbes have been found to influence a variety of neurological processes; one of the more notable connections is that of the flora to stress response. A common result of chronic stress, anxiety, or depression is the disruption of the intestinal barrier, which causes it to leak bacteria into the body cavity – a dangerous condition known as sepsis. This frightening problem has successfully been reversed in mice through administration of probiotics, notably one bacterium Lactobacillus farciminus. A gut shored up with healthy microbes may prove more resilient to stress-induced leakage in the first place.
Just two months ago, the high-profile journal Cell published a team's research on a possible connection between gut microbes and autism. Mice with symptoms similar to autism – avoidance of other mice, anxiety, and repetitive behaviors – were “cured†of these symptoms when fed the bacterial species Lactobacillus reuteri. These mice also showed an increase in oxytocin levels and increased neural circuitry in parts of the brain implicated in social interaction.
Autistic individuals commonly present with gastrointestinal problems such as inflammatory bowel disease and food allergies, and broadly the microbiome of autists has been found to be significantly different to that of non-autists.
Much research remains to be done, and results for mice do not equate to results for humans. Nevertheless, the importance of the body's relationship with its gut flora is now coming to light. The little menagerie we keep in our stomach has greater control over our weight, our mood, and our overall health than we ever could have imagined.
 Ruby Harrison is a Ph.D. graduate student in the Department of Entomology at the University of Georgia. Ruby studies endocrinology and reproduction of the yellow fever mosquito, Aedes aegypti – the same species that spreads Zika virus. In her free time she enjoys backpacking, camping, swing dancing, and cooking dumplings. Contact her at reh21923@uga.edu.More from Ruby Harrison. Ruby Harrison is a Ph.D. graduate student in the Department of Entomology at the University of Georgia. Ruby studies endocrinology and reproduction of the yellow fever mosquito, Aedes aegypti – the same species that spreads Zika virus. In her free time she enjoys backpacking, camping, swing dancing, and cooking dumplings. Contact her at reh21923@uga.edu.More from Ruby Harrison. |
About the Author
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 17, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 12, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 3, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/March 30, 2020