Are you a fan of hand sanitizer? Clorox wipes? When it comes to household cleanliness, most Americans are of the opinion that the fewer germs present, the better. And despite increased warnings of potentially dangerous consequences such as antimicrobial resistance, antimicrobial soaps, gels, wipes, and sprays continue to make up a large portion of America's cleaning routine. In fact, several recent studies have confirmed that triclosan and triclocarban, two potent antimicrobial agents, can be detected in up to 75 percent of Americans' urine and in up to 60 percent of our rivers and streams. In other words, in terms of hygiene, America is about as spotless as it can get.

However, antimicrobial resistance isn't the only phenomenon that could emerge from the developed world's love of all things squeaky clean. Recently, scientists have begun to ask whether living in a largely germ-free environment can impact health in other ways. As early as 1989, physicians and researchers alike noticed that as the developed world became more ‘clean' (i.e. as fewer people suffered from germ-causing infectious diseases), the incidence of other, non-infectious diseases (think: asthma, allergies) steadily rose.
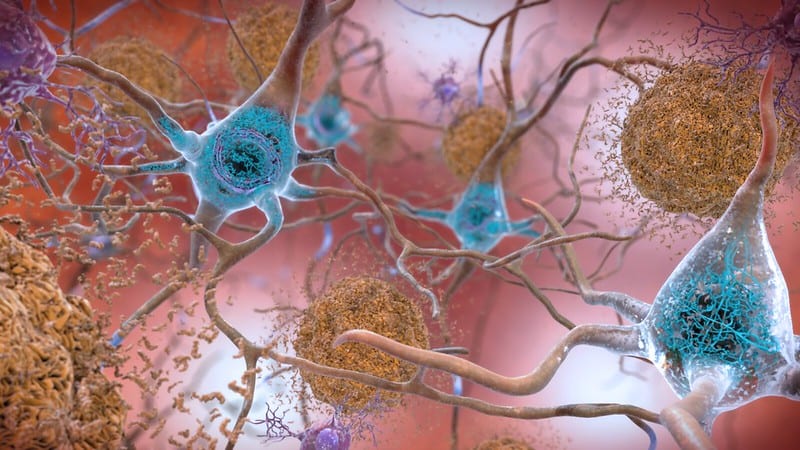
They proposed exposure to germs and germ-related toxins from the environment prepares one for illness in two ways. First, it allows an individual to build up defenses against a diverse array of microbes, like harmful bacteria, viruses, and parasites. Second, germ exposure might actually prepare one's immune system in such a way that the body learns to use its most lethal germ-killing tool, inflammation, only when dangerous bacteria, viruses, or parasites are present. Without this preparation, the body never learns a ‘threshold level' of tolerance to germs and the result is the chronic inflammation characteristic of diseases like asthma, allergies, arthritis, and more. This notion has come to be known as the hygiene hypothesis.
Following these observations of increased inflammatory disease incidence, scientists looked for ways to test and confirm this hygiene hypothesis, but it was a difficult situation to model. Finally, in 2016, Beura and colleagues from the University of Minnesota stumbled upon a great model seemingly by accident.
Beura and colleagues weren't trying to address the hygiene hypothesis. They were simply trying to alert the scientific community that mice raised in sterile laboratory conditions are not actually the ‘gold standard' model for human immunity they were previously considered. To do this, they measured characteristics of immune function in two groups of mice of the same species. One group had been raised in a sterile laboratory environment while the second group had been raised in a relatively ‘dirty' pet store. Then, they housed both groups together and looked at how the animals' immune systems changed.

The results were drastic. So drastic that 22 percent of the laboratory mice did not survive the exposure to the ‘dirty' mice. However, the laboratory mice that did survive displayed profound positive changes in immunity and were better able to withstand infection with dangerous bacteria.
This study introduced ‘dirty' and ‘clean' mice as a potential model for future hygiene hypothesis studies, but it did not answer an important question: Why did the laboratory mice die? Were they simply unable to mount an immune response to the germs carried by the ‘dirty' mice, or were they producing too much dangerous inflammation?
Another study by Abolins and colleagues at the London School of Hygiene and Tropical Medicine hints at the answer. Immune systems of mammals have two basic parts. The first part, the innate immune system, does not discriminate; it aims to kill potentially harmful germs as quickly as possible. For this reason, it is often known as the body's ‘first line of defense'. The more selective adaptive immune system can then identify, destroy, and remember specific germs. As it turns out, wild mice are much more equipped in their ability to quickly destroy dangerous germs than laboratory mice of the same species. These wild mice rely on strong innate immune responses. However, laboratory mice are more adept at mounting germ-specific inflammation via adaptive immunity. Low germ exposure essentially results in lab mice ditching a good portion of their first line of defense. This can leave them vulnerable to fast-acting infections, like the mice that died when cohabiting in Beura's study. However, the “over-preparedness†of their adaptive immune systems might cause them to mount inflammation in response to things that aren't actually dangerous, like allergens or even their own cells.
The take home? Germs may be good for you, at least to an extent. Nobody likes a dirty home, but the next time you're fishing through your closet for cleaning supplies, maybe reconsider using those Clorox wipes on your countertop. Your immune system will thank you.
About the Author
 Jenn is an MS student in the Department of Infectious Diseases at the University of Georgia, where she studies immune trade-offs in tissue-regenerating rodent species. Jenn loves to dance, draw, hike, and demolish large quantities of food in her spare time. She's also in love with dogs and spends plenty of time with her pampered pooch, Ziggy. Feel free to check out a few of her ASC poster designs, personal research website, or to contact her at jennifer.cyr25@uga.edu or on Twitter at @jennlcyr! Jenn is an MS student in the Department of Infectious Diseases at the University of Georgia, where she studies immune trade-offs in tissue-regenerating rodent species. Jenn loves to dance, draw, hike, and demolish large quantities of food in her spare time. She's also in love with dogs and spends plenty of time with her pampered pooch, Ziggy. Feel free to check out a few of her ASC poster designs, personal research website, or to contact her at jennifer.cyr25@uga.edu or on Twitter at @jennlcyr! |
About the Author
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 17, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 12, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 3, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/March 30, 2020