My heart skips a beat everytime I read about new technologies that could have saved my brother's life. My brother passed away last year due to complications from congestive heart failure. A heart transplant could have possibly saved his life, but it's well known that the demand for organ transplants in this country far outweighs the supply.
According to the U.S. Government's Information on Organ Donation and Transplantation, there are over 116,000 people on the national transplant waiting list. It's daunting to realize that a new person is added to that list every 10 minutes; and on average, 20 people die each day while waiting for a match. The first human heart transplant was conducted in Cape Town, South Africa almost 50 years ago to the date of this publication.

Since then, organ transplantation has seen some amazing technological advances, but none effectively address the issue of the number of patients far exceeding available donor organs. What if technology existed so that nobody had to wait for a matching donor for an organ to become available? What if a viable replacement organ could always be ready, whenever and wherever, it was needed? What if there was no longer a need for human organ donors?
Scientists are actually looking towards the barnyard to find a suitable substitute! Turns out, pigs could be an ideal candidate for human organ transplant. Certain pig organs are similar enough in size and function to be used as replacements for defective or damaged human organs. The process of using animal tissues for human transplantation is called xenotransplantation. It's already performed, but only with non-living tissue types. For example, pig aortic valves can be used when a person experiences valve failure–my dad actually underwent this surgery in his 50s. Unfortunately, most pig organs are not considered suitable for transplant because the living tissue may contain retroviruses that are specific to pigs. While scientists are not sure if these viruses could be harmful to humans, the risk of transmission and uncertainty of infection leaves xenotransplantation tightly regulated.

A recent breakthrough by researchers at Harvard may have put pig back on the menu for awaiting transplant patients. Using advanced gene editing technology, they have discovered a way to remove all of the potentially harmful retroviruses from the entire pig genome. The genetically modified pigs are healthy and grow to the optimal size so that their organs are comparable to human organs.There are still other factors that need to be addressed in order to make the pig organs “humanized†enough for successful transplantation, but researchers are optimistic that this is a big step in the right direction. And even though more research can be done to address any safety concerns as this technology moves forward, there are still ethical concerns surrounding the use of xenotransplantation. Certain animal rights groups have condemned the use of animals for organ transplant and for scientific research in general. There are also individuals who would be opposed to xenotransplantation for religious reasons. This could be a particular issue within the Muslim and Jewish communities; however, many agree that the use of these transplants could be acceptable within certain circumstances, such as life or death situations.
Considered a radical surgical procedure only 50 years ago, human organ transplants are now done around the world, with it's main limitation being the lack of suitable organs. Attempts at xenotransplantation have been made over the decades, but the risks and challenges stalled success. The technological advances now available in xenotransplantation pave the way for an unlikely farm animal to solve the major problem of organ shortage. While my brother may not have been fortunate enough to benefit from these phenomenal medical advances, the hope remains for thousands of patients in the U.S. alone.
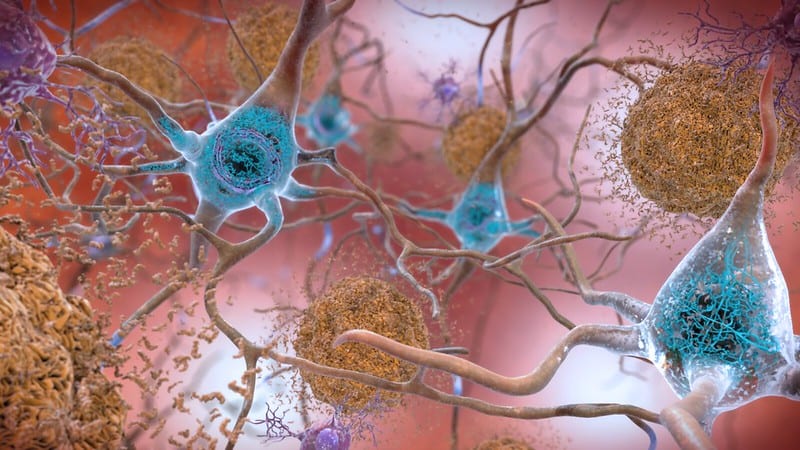
Featured Image Credit: Paul Cross via Flikr
 Michelle Dookwah is a graduate student at the University of Georgia Complex Carbohydrate Research Center, where she studies rare neurological disorders using patient stem cells. She's pretty passionate about science and science communication. However, she also enjoys numerous activities in her free time, including reading, listening to podcasts and audiobooks, hiking, baking, and obsessing over her labradoodle named Goose! More from Michelle Dookwah.
Michelle Dookwah is a graduate student at the University of Georgia Complex Carbohydrate Research Center, where she studies rare neurological disorders using patient stem cells. She's pretty passionate about science and science communication. However, she also enjoys numerous activities in her free time, including reading, listening to podcasts and audiobooks, hiking, baking, and obsessing over her labradoodle named Goose! More from Michelle Dookwah.
About the Author
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 17, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 12, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 3, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/March 30, 2020