One fact that was drilled into my head while studying biomedical science was how few experimental drugs ever make it past clinical trials. A failure rate of 90% is reported. This struck me as odd, but I chalked it up as an example of how difficult drug development is and didn't ask why. That changed when I decided to use mice as part of my thesis project. Initially reluctant, my graduate advisor convinced me it would be the best way to prove my hypothesis. As my experiments progressed, though, I started to wonder if the mice on my lab bench could really predict how a human would respond to the same treatment. This led to discoveries that would completely change my outlook on preclinical drug testing.

Ultimately, the reason so many drugs fail clinical trials comes down to two pillars of biomedical science: safety and efficacy. If a drug has dangerous side effects or if it doesn't provoke a therapeutic response in enough people, it's thrown out. As part of the preclinical regulatory process, the Food and Drug Administration (FDA) mandates that any investigational drug compound must be extensively tested in at least a few different species before approving it for clinical trials. To better understand why that is, it's useful to examine the medical tragedy happening as the legislation was passed.
In the late 1950s and early 1960s, the world was reeling from the discovery that a new sleeping pill, thalidomide, would cause severe birth defects when taken by pregnant women. Developed and marketed in 1957 by the German-based company Chemie Grünenthal, it is estimated that over 15,000 children worldwide were born with deformities linked to thalidomide. The US, however, was mostly spared due to the FDA's refusal to approve the drug. Politicians such as Senator Estes Kefauver (D-Tennessee) criticized Grünenthal while praising the FDA for recognizing the potential danger. Surely, the whole tragedy could have been prevented if the company simply tested their drugs on pregnant animals! In 1962, the Kefauver Harris Amendment to the 1938 Federal Food, Drug, and Cosmetic Act was passed, mandating that new drugs had to be proven safe and effective before being administered to humans. Extensive animal testing was enforced as the gold standard of ensuring this.
Here's the thing: no one knows if Grünenthal actually tested thalidomide on pregnant animals. All of their records were destroyed. What we do know is that teratogenicity (embryonic toxicity) testing was routine by the 1950s. It's unlikely that a well-established pharmaceutical company would just not perform those tests, but let's assume they didn't. Would more animal testing have prevented the disaster? To answer that, consider Karnofsky's law:
Any drug administered at the proper dosage, and at the proper stage of development to embryos of the proper species…will be effective in causing disturbances in embryonic development.

Extensive animal testing has proven this to be true. By 2004, 1500 drugs had been shown to produce birth defects in at least one animal species, while only 40 were known human embryonic toxins. Mice and most other rodents do not exhibit classic thalidomide toxicity, even at doses of 4000 mg/kg. (In humans, thalidomide typically produces birth defects at 0.5 mg/kg!) Only monkeys consistently experienced birth defects when given thalidomide, and then only at 10 times the usual human dose. Unfortunately, this turned out to be an exception rather than the rule. For other known human embryotoxins, the value of using toxicity in non-human primates to predict human toxicity is very low. So, with all of these divergent results using modern techniques, would it seem likely that 1950s scientists could have been able to make sense of more animal data?
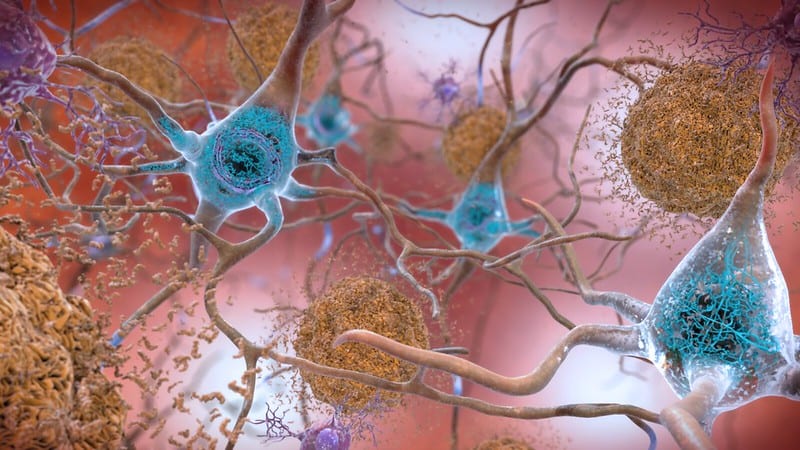
Animals are not little humans. Biological systems are so complex that even if two species share almost all of the same genes, the way that those genes are regulated and how they interact with each other can lead to totally different outcomes. Animal models routinely fail to predict safety and efficacy in humans, despite that being the very measure they are supposed to assess.Imagine how many potentially life-saving drugs have been discarded based on poor results in animals! It's clear to me that the FDA needs to revisit Kefauver Harris, but what can be done in the absence of reliable alternatives to animal testing?
Stay tuned for part 2 of this series, where I will go over current efforts to phase out animal testing in preclinical drug research.
About the Author
 Israel Tordoya is an MS student in the Department of Pharmaceutical and Biomedical Sciences, studying the relationship between obesity and breast cancer. One day, he hopes to be an advocate for marginalized people (and animals!) in medicine while developing generic drugs. In his free time, he likes to run, listen to audiobooks, and make bad music. Find him on Twitter: @TordoyaIsrael or email him: it37190@uga.edu
Israel Tordoya is an MS student in the Department of Pharmaceutical and Biomedical Sciences, studying the relationship between obesity and breast cancer. One day, he hopes to be an advocate for marginalized people (and animals!) in medicine while developing generic drugs. In his free time, he likes to run, listen to audiobooks, and make bad music. Find him on Twitter: @TordoyaIsrael or email him: it37190@uga.edu
About the Author
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 17, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 12, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 3, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/March 30, 2020