Although rewriting the code of life seems like a daunting task, scientists have managed to do just that. You've probably heard of CRISPR technology, a burgeoning genetic tool that has seen use in a multitude of applications, from treating Duchenne muscular dystrophy in mice to making crops more sustainable. The technology offers a method of editing DNA, the string of four bases (A, T, C, and G) that makes up the script of a living organism.
How does CRISPR work?
CRISPR (short for clustered regularly interspaced short palindromic repeats) consists of two parts: Cas9, a pair of molecular ‘scissors' that cuts DNA, and single guide RNA (sgRNA), a template that guides Cas9 to the desired section of DNA. These two components, abbreviated CRISPR-Cas9, work in two stages. First, the sgRNA finds its string of bases in an organism's DNA. It can do this because bases in sgRNA and DNA pair together using two rules: A goes with T, and C goes with G. Then, Cas9 makes a break in the string of DNA at that location. CRISPR can target any string of 20 bases.
CRISPR is exciting to many researchers because of how accurately it can be guided to cut DNA. Researchers often want to target genes, the pieces of DNA that encode instructions for proteins. By altering a gene, researchers can see what effects it has on the organism, giving clues as to how it works. Before CRISPR, scientists used technologies that did the docking and cutting steps in one part, making targeted gene editing more complex and risky. They also risked cutting sequences that were similar, but not identical to, the actual sequence they wanted to target. In comparison, CRISPR can successfully target 60% of cells when used to replace defective genes and achieve 99.9% accuracy with further modifications. Consequently, this technology's promise has grown well beyond the lab and into a new form of medicine.

Breakthroughs in treating genetic disorders
CRISPR is a potential therapy for an entire class of disorders. In genetic disorders, the gene encoding some protein is faulty, causing it to work less efficiently, or not at all. If researchers provide a working copy of the gene alongside the CRISPR-Cas9 machinery, they can permanently replace the faulty copy for a functional one. Ideally, this gene ‘swap-out' occurs without altering unrelated parts of a person's DNA.
Huntington's disease is one such example. In this condition, a mutation (a ‘typo' in the DNA) encoding a protein called huntingtin is present. This produces a lengthened huntingtin mutant, and in mouse models, the mutated huntingtin is chopped into pieces, forming clumps in the brain that prevent nerve cells from working properly. CRISPR-Cas9-based treatment has been shown to reduce the formation of these clumps, with no detectable effect on the DNA surrounding the huntingtin gene.
Treatment of sickle-cell disease with CRISPR has shown even more promise. Here, an oxygen-carrying protein, hemoglobin, is mutated. This mutated hemoglobin accumulates into fibers that deform red blood cells, resulting in organ damage. In the CRISPR treatment, a copy of DNA encoding functional hemoglobin was given to a sufferer of this condition, Victoria Gray, in a clinical trial. One year since, she has reported great health and has appeared to recover significantly.
Embryo research and limitations of CRISPR therapy
Whereas CRISPR therapy in adults has shown promise, applying the technology to embryos, called germline editing, has been highly controversial. The example of Dr. He Jiankui highlighted this controversy—he modified two embryos, named Lulu and Nana, from a couple where one partner was HIV-positive. Using CRISPR, Jiankui altered the DNA encoding CCR5, a protein used by HIV to infect cells. CRISPR makes a cut in the CCR5 gene, inactivating it and, in theory, making cells unsusceptible to HIV infection.
The use of CRISPR in embryos led to concern in the scientific community, with many worrying about off-target effects. Although Jiankui claims only CCR5 was targeted, was it really? It has been shown that sgRNA can misguide Cas9 to sequences where the ends are mismatched. Furthermore, CCR5 might play a role in protecting from other viral infections. Current updates on the health of Lulu and Nana (and the status of Dr. He Jiankui) remain scant, so it remains unclear whether the therapy has had any negative effects.
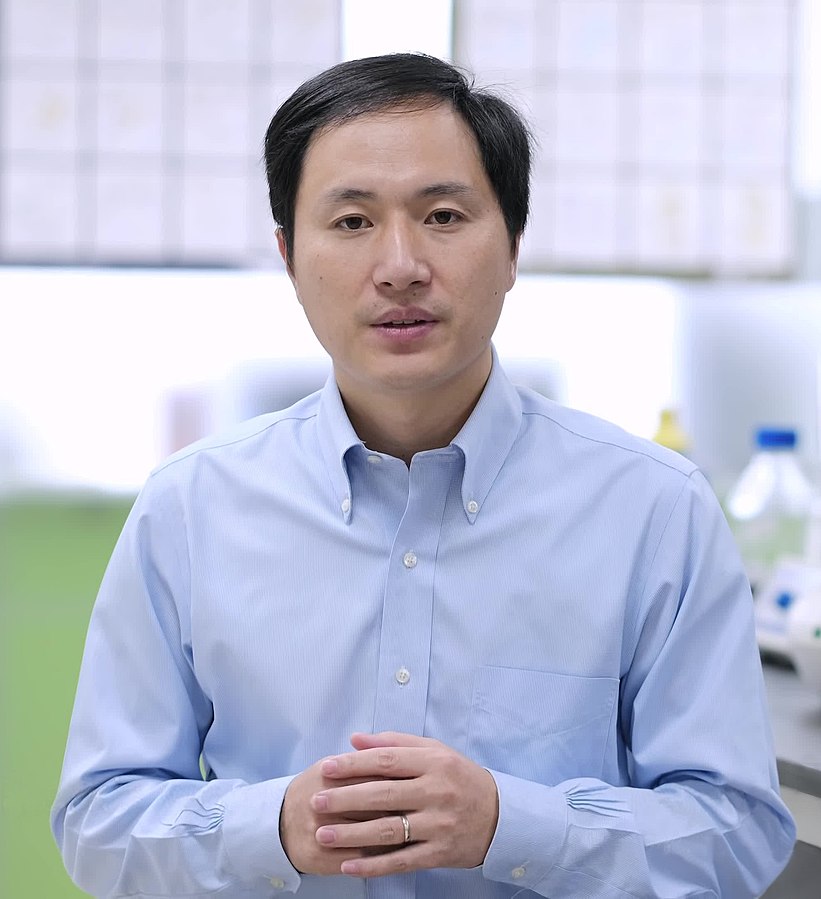
Fears about the use of CRISPR in embryos range from those of broader misuse to make ‘designer babies' to more fundamental ones about the effects of large DNA deletions. Other studies have shown that CRISPR-edited embryos can have large rearrangements and deletions in their chromosomes, the packages of DNA within the cell. Certainly, the treatment of embryos could eradicate a genetic defect for good, but it could also have unknown effects that linger on in future generations. For now, the use of CRISPR technology in embryo research remains tightly banned, at least until a more robust and efficient version becomes viable.
The future of CRISPR therapy
CRISPR is a promising gene editing and therapy tool—in both animals and humans, it has been shown to treat genetic disorders for which there is currently no cure. As a highly versatile technology that's been recognized in the 2020 Nobel Prize in Chemistry, it's only a matter of time before we see it in the clinic. With that said, CRISPR still faces some hurdles, both with how accurate the technology is itself, as well as how scientists are allowed to use it. The impact of CRISPR in medicine is clear, yet how we choose to edit the code of life is a future that only we can write.
Featured image: “CRISPR Cas9” by “National Human Genome Research Institute” is licensed under CC BY-NC 2.0.
About the Author
- Kaito Nagashimahttps://athensscienceobserver.com/author/kaito-nagashima/October 27, 2022
- Kaito Nagashimahttps://athensscienceobserver.com/author/kaito-nagashima/October 27, 2021