After taking a trip back in time to learn the history of vaccines and then inside a vaccine to learn the ingredients, we continue Vaccine 101 with our next lesson: why vaccinate?

As a 90's baby, I have been fortunate to never see first hand the tragedy caused by diseases such as polio, measles, or whooping cough. My parents did not worry about whether or not I would contract these diseases thanks to vaccinations. Because of widespread vaccination in our country, these diseases are rarely seen in the United States, but they are still prevalent in other countries, and can still infect children in the United States when the opportunity arises. Today we see a lot of debate surrounding vaccines and whether or not to vaccinate. Let's walk through why vaccination is important and essential to a healthy society.
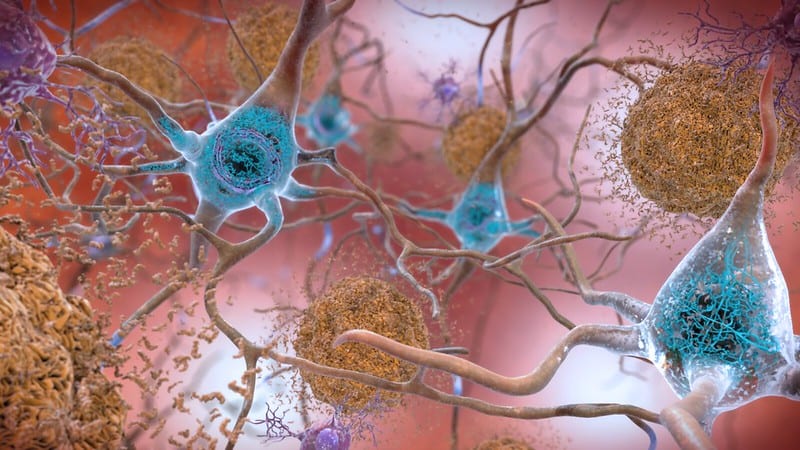
Vaccination and Personal Immunity
To most, the obvious reason to vaccinate is for personal protection. By vaccinating yourself, you are providing long-term, sometimes lifelong, protection against a disease. This can help to protect you against disease in your own country as well as those you may encounter while travelling abroad. Diseases like yellow fever are not a common occurrence in the United States, but they are still prevalent in some parts of South America and Africa. Unfortunately, Disease does not stop at the border, but can be carried in from abroad. In 2014 the U.S. experienced a multistate measles outbreak linked to an amusement park in California. The outbreak was attributed to a traveler who became infected while overseas, most likely in the Philippines. Thanks to vaccines you can protect yourself from these diseases at home or abroad.
Vaccination and Herd Immunity

Vaccination doesn't just benefit you alone, however. Individual vaccination helps protect your neighbors by contributing to herd immunity, sometimes referred to as community immunity. For various reasons some individuals, such as newborns and those with chronic illness, cannot be vaccinated. The herd immunity of a community with a high vaccination rate protects these individuals, while reducing the likelihood of outbreaks. This occurs because a disease-causing organism, like the measles virus, has a more difficult time gaining a foothold when most people are already immune to it. Think of herd immunity like a castle; the castle walls prevent invaders from reaching inside the castle because they can't find a way to infiltrate the walls. If no one is vaccinated, then you have no walls; the invader can easily enter. If you have high vaccination rate in a community you build higher castle walls, breaking the chain of human transmission and preventing the disease from entering, protecting those who are unvaccinated.
The key to effective herd immunity is that vaccination rates within a community must reach a certain level, or threshold. If this level is not met disease outbreaks can still occur. Different diseases require different vaccination levels, but how is this determined? Disease characteristics, the population, and vaccine effectiveness are all factors used to determine the minimum percentage of individuals that must be vaccinated to have herd immunity.
Epidemiologists, experts in infectious disease transmission, can determine a “basic reproduction number†for a disease. This number represents the number of people in an unprotected population who would “catch†the disease from a single infected person. Basically, how infectious is each disease? If I am infected with measles I could pass it to 12-18 people, but if I was infected with polio I would only pass it to 5-7 people. Why are these numbers so different?
When an individual with measles sneezes or coughs, the virus spreads through the air, where it can remain for up to 2 hours. On the other hand, polio spreads through fecal contamination of water or food that is then eaten. These different types of transmission from person to person allow measles to spread more easily than polio. When looking at a population, certain diseases such as pertussis (whooping cough) can also have more severe consequences for specific groups. Pertussis is severe at all ages but infants have the highest death rate from the disease. All of these factors must be taken into consideration to determine what percentage of individuals in a given population must be vaccinated to have effective herd immunity.
For a fast spreading disease like measles the required vaccination rate is 95%. In the 1990's in England vaccination for measles, by the MMR vaccine, dropped below this threshold to 80%. Measles cases began to rise from 56 cases in 1998 to 1,348 in 2008. Despite halting the spread of measles more than a decade prior, this disease once again became a common occurrence due to the decreased vaccination rates. For a disease like polio 80% of the community needs to be vaccinated to create effective herd immunity. Just as higher vaccination rates raise the castle walls, as vaccination rates drop the walls become shorter and shorter, until the invading disease can again gain a foothold.
In this Vaccine 101 lesson you have learned that vaccination is not only important for the protection of yourself but also others. When individuals get vaccinated they help to protect those who can't, by putting up castle walls and keeping the invaders out. Before vaccines were created, diseases like smallpox, measles, and polio were common horrors looming over society, ready to strike. Routine vaccination has kept these diseases at bay; it has built higher castle walls, and allowed us to no longer fear them. When you break the route of human-to-human transmission you interrupt the likelihood of disease outbreak. Thorough vaccination can even succeed in worldwide disease eradication, as we've accomplished with smallpox and are working towards with polio. To learn more about global vaccination efforts join me for the next Vaccine 101 post!
About the Author
 A native Virginian (GO HOKIES!), Caitlin Reeves is a PhD candidate in the Microbiology department studying attachment of the human respiratory pathogen Mycoplasma pneumoniae to its human host. Outside of the lab she can be found planning events for UGA's Women in Science (WiSci) organization, snuggling with her labradoodle Sherlock, or playing video games despite being a 26 year old “adultâ€. A native Virginian (GO HOKIES!), Caitlin Reeves is a PhD candidate in the Microbiology department studying attachment of the human respiratory pathogen Mycoplasma pneumoniae to its human host. Outside of the lab she can be found planning events for UGA's Women in Science (WiSci) organization, snuggling with her labradoodle Sherlock, or playing video games despite being a 26 year old “adultâ€. |
About the Author
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 17, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 12, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 3, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/March 30, 2020