If we accept the idea that animal models are holding back drug development due to a potential inability to predict safety and efficacy in humans, what can be done to fix it? Increasingly, scientists are using human cells cultured in vitro to assess the safety and efficacy of new drug compounds. While in vitro cell cultures have absolutely reduced the number of animals that are used in drug testing, it is clear that cells in a petri dish behave a lot differently than the cells that make up our bodies.
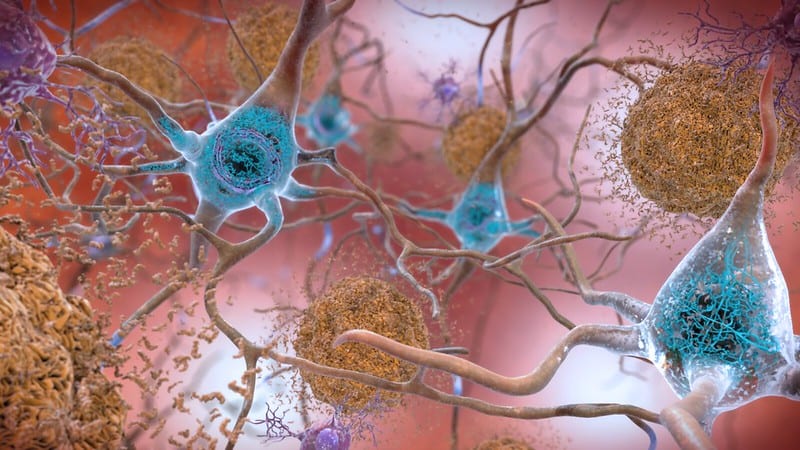
The cells in our bodies are suspended in a network of structural and biochemical support molecules called the extracellular matrix. They grow in 3 dimensions, and any particular area can have a huge variety of different cell types. Drugs are delivered to and taken from the cells in our body through blood vessels, and there is a barrier between the blood vessel wall and the underlying tissue that makes it more difficult for drugs to get to where they need to go. Compare that to cells in a petri dish, where a single type of cell grows on a 2-dimensional plane. To test a drug, you mix it into the culture medium and let the cells soak in it. Given all of this, is it any wonder that a scientist would want to see how their drug works in a whole organism?
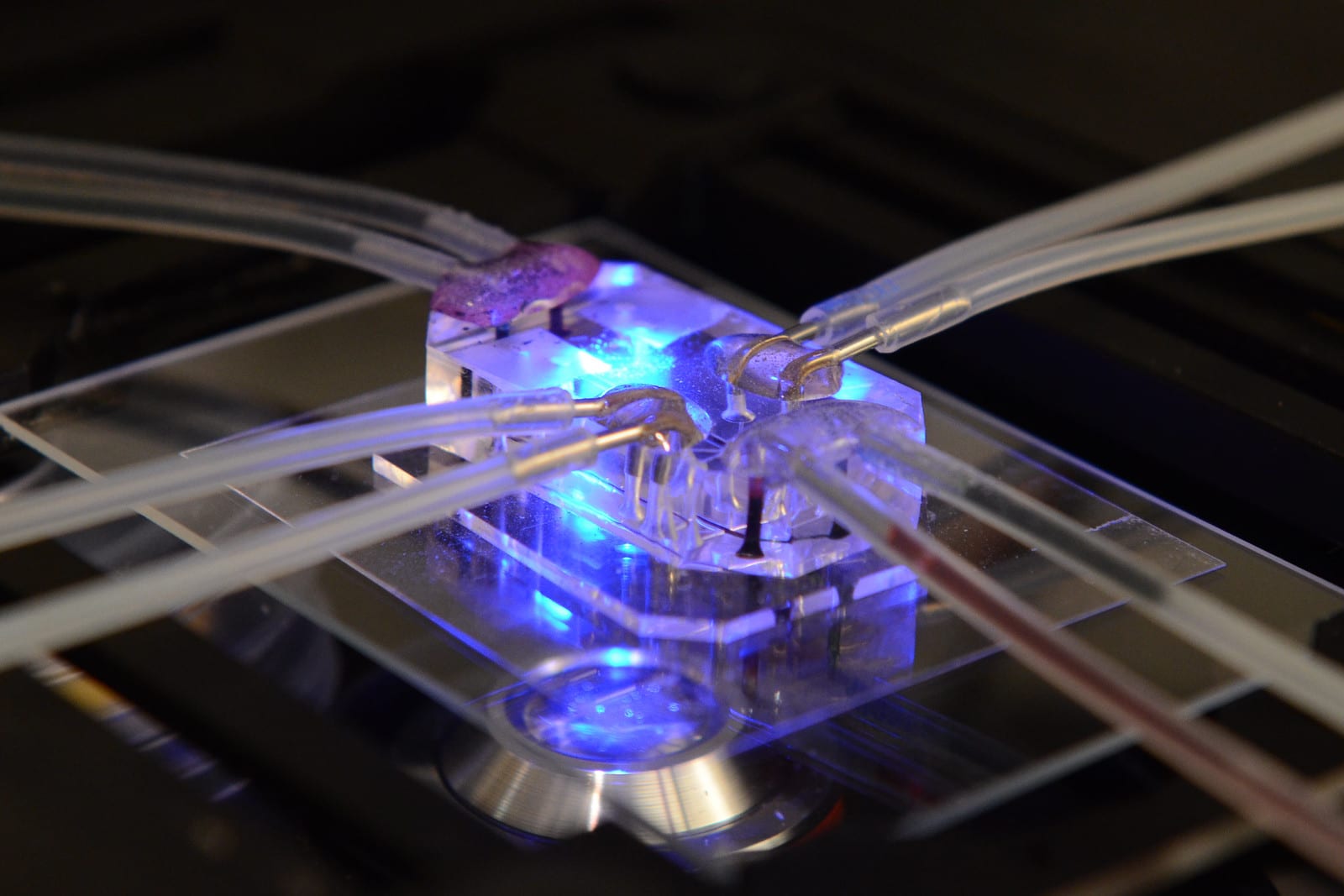
In vitro biological models have come a long way since cell culturing techniques were first developed. Clever engineering is used to grow cells in 3D scaffolds, or multiple types of cells separated by permeable membranes. What if an in vitro system was engineered to model all of the essential characteristics of drug delivery to human cells? In Jan 2009, Harvard's Wyss Institute for Biologically Inspired Engineering was founded by Donald Ingber and one of the first projects he undertook was to come up with a better way to test drugs. By using techniques adapted from computer microchip manufacturing, they were able to develop microchips containing living human cells. These “organ chips†are poised to revolutionize drug development by replicating all of the critical characteristics of drug delivery to a particular organ.
To understand how organ chips work, it's best to look at the first one that was developed. The human lung alveolus chip is about the size of a flash drive, with three parallel channels going along its length. The central channel is divided into top and bottom halves by a semipermeable membrane. The top is lined by lung alveolar cells, while the bottom chamber is lined by cells from the blood vessels in the lung. The top chamber is filled with air and the bottom chamber is filled with some liquid medium (that can even be whole human blood). The two remaining chambers are hollow, and a vacuum can be cyclically applied to them to stretch the membrane in the central chamber and mimic “breathingâ€. One can imagine a scientist using this lung chip to test an inhaled drug by pumping the drug into the air chamber and seeing how well it's absorbed across the membrane into the “bloodâ€.
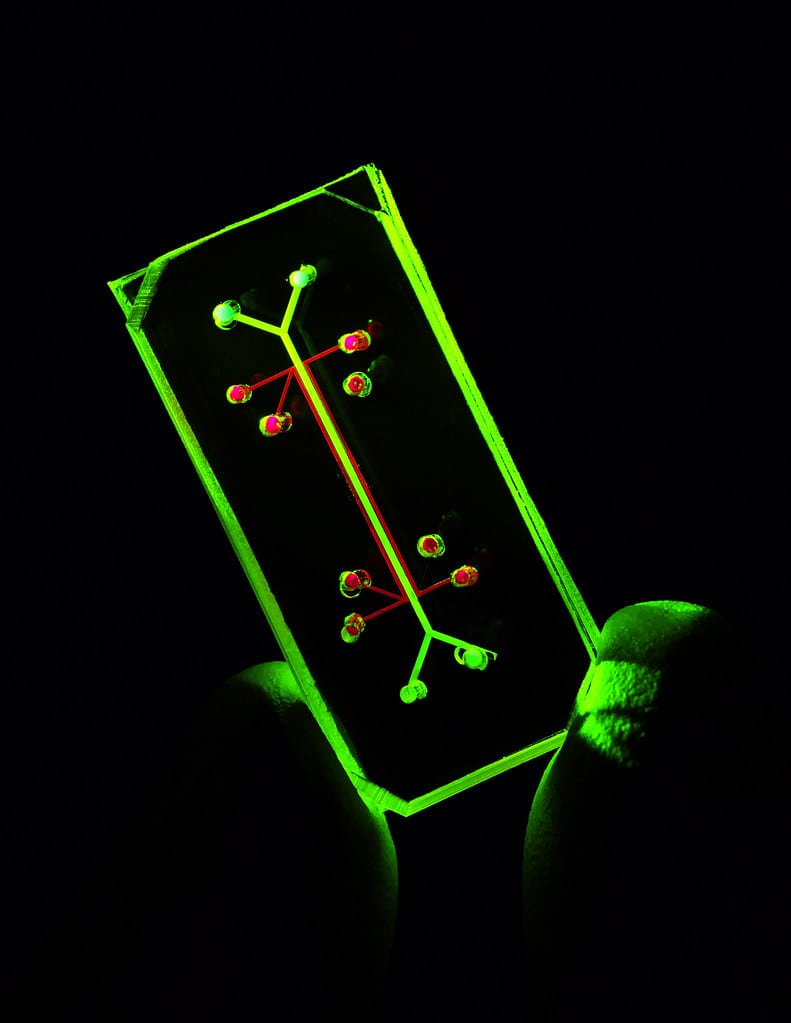
Why stop there? If you have a chip for each major human organ, it's totally possible to link them all together and make an integrated “human-body-on-a-chipâ€. Such a model system would allow for pharmacokinetic and pharmacodynamic analysis of a drug without ever giving it to a living organism. That's the goal of Emulate Inc., Donald Ingber's biotech startup built on his work at the Wyss Institue. In order for this technology to leave academic labs and become a part of industrial drug development, their so-called “Human Emulation System†has to be turned into a user-friendly product. Furthermore, manufacturing has to be consistent, and the FDA has to work with them to develop standard protocols for each type of test. They have to empirically demonstrate that this technology predicts human drug responses better than animal models before the FDA will allow it to stand in for animal testing.
The story of organ chips is illustrative of how biology can be used to inform the design of new technologies. Beyond just saving the lives of research animals, organ chips have the potential to dramatically increase the quality of drug development and improve patient health outcomes.
About the Author

Israel Tordoya is an MS student in the Department of Pharmaceutical and Biomedical Sciences, studying the relationship between obesity and breast cancer. One day, he hopes to be an advocate for marginalized people (and animals!) in medicine while developing generic drugs. In his free time, he likes to run, listen to audiobooks, and make bad music. Find him on Twitter: @TordoyaIsrael or email him: it37190@uga.edu
About the Author
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 17, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 12, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/April 3, 2020
-
athenssciencecafehttps://athensscienceobserver.com/author/athenssciencecafe/March 30, 2020